Author: Building Trust
How to build trust at your organization

Is your institution trying to rebuild trust, but you don’t know where to start? Or do you have success stories that would help others learn, but don’t know how to share them?
The ABIM Foundation’s Building Trust initiative was created to increase conversation, research and best practices to elevate trust as an essential organizing principle for improving health care. Health care leaders spoke about their efforts to build trust at their organizations. Micah T. Prochaska, MD, MSc, FHM, Assistant Professor of Medicine at the University of Chicago, Donna Cryer, JD, President & CEO of the Global Liver Institute, and Daniel Wolfson, MHSA, Executive Vice President & COO of the ABIM Foundation, discussed the tools they used, challenges they faced, and the successes they saw.
Read Donna Cryer’s blog post: Trust that we won’t go back
Previous Webinars:
- Conversation Series: Distributed, decentralized and digitally-enabled care
- Public Agenda is building trust with patients
- Conversation Series: COVID-19’s impact on trust
- Introducing the Building Trust Initiative
- Vaccine hesitancy impacts on state and local vaccine planning
- Enhancing Influenza and COVID19 caccine uptake
- Tools for building institutional trust
- The evolving role of Community Health Workers as trusted messengers
Building trusting relationships by using the right language
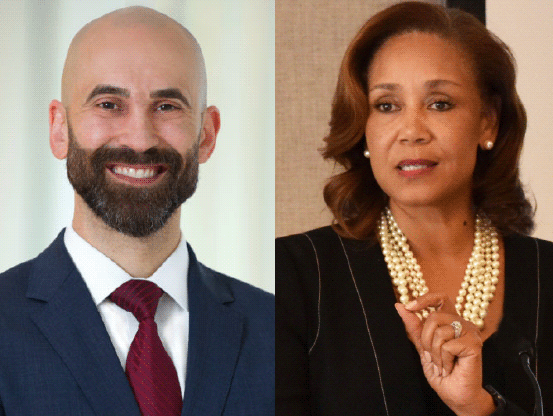
Philip Alberti, PhD, Founding Director of the Association of American Medical Colleges (AAMC) Center for Health Justice, and Pamela Browner White, Chief Diversity, Equity and Inclusion Officer and Senior Vice President of Communications at ABIM and the ABIM Foundation, discussed the AAMC’s new Center for Health Justice, which was created in 2021 to address health inequities and improve community health across the US.
Philip also offers insight into the newly developed health equity communication guide, which was published jointly by the AAMC Center for Health Justice and the American Medical Association to support clinicians’ conversations with patients. The comprehensive guide promotes a deeper understanding of equity-focused, first-person language and why it matters. Philip and Pamela discussed why this language is so important in building trusting relationships and its impact in delivering equitable care for all.
Clips
Previous Webinars:
- Conversation Series: Distributed, decentralized and digitally-enabled care
- Public Agenda is building trust with patients
- Conversation Series: COVID-19’s impact on trust
- Introducing the Building Trust Initiative
- Vaccine hesitancy impacts on state and local vaccine planning
- Enhancing Influenza and COVID19 caccine uptake
- Tools for building institutional trust
- The evolving role of Community Health Workers as trusted messengers
Learning Network Webinar Series: Providing support following a patient harm event
Thomas H. Gallagher, M.D., general internist, Associate Chair for Patient Care Quality, Safety, and Value, and Professor at the University of Washington, and Carole Hemmelgarn, MS, MS, Senior Director of Education for the MedStar Institute for Quality & Safety, and Senior Director for the Executive Master’s program for Clinical Quality, Safety & Leadership at Georgetown University discussed how UW Medicine’s Communication and Resolution Program (CRP) seeks to provide support for patients, families, and involved clinicians following a patient harm event by promoting empathic, transparent, and ongoing communication about what happened and what patients and families most need in its wake.
- Conversation Series: Distributed, decentralized and digitally-enabled care
- Public Agenda is building trust with patients
- Conversation Series: COVID-19’s impact on trust
- Introducing the Building Trust Initiative
- Vaccine hesitancy impacts on state and local vaccine planning
- Enhancing Influenza and COVID19 caccine uptake
- Tools for building institutional trust
- The evolving role of Community Health Workers as trusted messengers
ABIM Foundation and the Institute for Healthcare Improvement partner to build trust in US health systems
The organizations will use an evidence-driven approach to identify behaviors and practices that make health care providers and organizations more worthy of trust, with the goal of replication nationwide
PHILADELPHIA and BOSTON, November 22, 2021 – Trust at all levels of the health care system is at historic lows, affecting quality of care and equity among patients and communities. According to a survey released by the ABIM Foundation in May 2021, about one in every eight adults say they have been discriminated against by a US health care facility or office, with Black individuals being twice as likely to experience discrimination in a health care facility compared to white counterparts. That’s why the ABIM Foundation and the Institute for Healthcare Improvement (IHI) are partnering to identify and promote practices, policies, and behaviors for rebuilding trust in US health care systems.
IHI will spearhead an effort to assess the current landscape of trust in health care, including reviewing existing literature and conducting interviews with leaders and clinicians at health systems that have achieved high levels of clinician-patient trust. The findings will enable IHI to develop a clear set of actions health care systems can take to enhance trust between providers and the patients they serve, with a particular focus on strengthening relationships with communities of color.
This theory of change will incorporate and build on the system-level drivers of clinician-patient trust that the ABIM Foundation has identified as part of its work in this area: Competency, caring, compassion, comfort/equity, and cost.
“We launched the Building Trust initiative to elevate the importance of trust as an essential organizing principle to guide operations and improvements in health care, including promoting health equity,” said Richard J. Baron, MD, President and CEO of ABIM and the ABIM Foundation. “We’re well on our way of creating a vanguard community of organizations interested in addressing trust, and now is the time to build on this work and move toward deriving a specific set of trust-enhancing practices that can easily be spread across health care systems.”
“Rebuilding trust is critically important to our efforts to improve health and health care worldwide, and to addressing health equity in particular,” said Kedar Mate, MD, President and CEO of IHI. “Our hope is to build on this work by pilot-testing trust-building practices with a small group of US health care organizations, and eventually scale the effort across the country.”
###
About the ABIM Foundation
The ABIM Foundation’s mission is to advance medical professionalism to improve the health care system by collaborating with physicians and physician leaders, medical trainees, health care delivery systems, payers, policymakers, consumer organizations and patients to foster a shared understanding of professionalism and how they can adopt the tenets of professionalism in practice. To learn more about the ABIM Foundation, visit www.abimfoundation.org, connect on Facebook or follow on Twitter.
About the Institute for Healthcare Improvement (IHI)
The Institute for Healthcare Improvement (IHI) is an independent not-for-profit organization based in Boston, Massachusetts, USA. For 30 years, IHI has used improvement science to advance and sustain better outcomes in health and health systems across the world. IHI brings awareness of safety and quality to millions, catalyzes learning and the systematic improvement of care, develops solutions to previously intractable challenges, and mobilizes health systems, communities, regions, and nations to reduce harm and deaths. IHI collaborates with a growing community to spark bold, inventive ways to improve the health of individuals and populations. IHI generates optimism, harvests fresh ideas, and supports anyone, anywhere who wants to profoundly change health and health care for the better. Learn more at ihi.org.
Media Contacts
ABIM Foundation
Jaime McClennen, 609-703-6909
jmcclennen@abim.org
Institute for Healthcare Improvement
Joanna Clark, CXO Communication, 207-712-1404
joanna@cxocommunication.com
Building Trust in your primary care practice
Senior Investigator Michael Parchman, MD, MPH, of the MacColl Center for Health Care Innovation, part of Kaiser Permanente Washington, is a nationally recognized expert on applying implementation science to primary care. As both a family practitioner and health services researcher, he has more than 25 years of experience as a clinician and medical educator.
Building Trust team: Can you tell me why you think trust is important in improving health care and what interests you in the topic?
Dr. Parchman: This work began several years ago, when the Robert Wood Johnson Foundation approached us about the issue of engaging clinicians and other health care professionals in addressing overuse and promoting high value care. The more we explored this issue, the more we became aware of how trust is woven deeply into the fabric of every aspect of delivering high value care. It came up over and over again, and also came up repeatedly in our opioid work, where we are supporting primary care clinics in redesigning their care systems for patients who are on long-term opioids for chronic pain.
BT: You’re now working on a project that’s focused on medical management for dementia patients in ACOs. Can you tell us more about that project and how trust factors into the work?
Dr. Parchman: We’re currently funded by the IMPACT Collaboratory, which is a National Institute of Aging-funded initiative, to work with ACOs on prescribing potentially inappropriate medications for patients with dementia. This raises clear issues of trust with both patients and their family members or caregivers. For example, they may ask, “Why was I started on this medicine in the first place?” So, there’s a trust in the medical profession issue that arises.
Clinicians may also not trust data that’s presented to them about how often they prescribe these medications. Clinicians may not trust patients to follow through on replacement services that might be safer and sometimes more effective than some of the medications. And then there’s the issue of clinician and patient trust in the evidence behind the potential harm from these medications. Many clinicians say, “I know these studies show there’s potential for harm from these medications but they’re not like my patients.” Finally, as a clinician there’s trust in your organization to support you in decreasing the use of a service for which the potential for harm is greater than the benefit, and trusting your peers not to prescribe these potentially inappropriate medications.
BT: What do you hope to measure around trust with this project?
Dr. Parchman: We’re training 30 clinicians across two ACOs to become clinician champions. Through a curriculum and a project workbook, we’re going to partner with these clinicians to look at how they implement this work in their own setting and use the data they enter in the project workbook to discover how often issues of trust come up, what kinds of trust issues come up, and how they address them. (Find the workbook and curriculum at Taking Action on Overuse.)

BT: What have you learned about trust from your work on de-prescribing opioids and older adults?
Dr. Parchman: Our work focuses on six building blocks for opiate medication management. When clinics engage with our team, coaches or facilitators help them look at how they are managing opioid medications. Clinics sometimes come to us when they unexpectedly find themselves inheriting patients who have legacy opioid prescription from a retiring provider. When those patients come in for refills, there’s that difficult conversation about why they are on the medication and the potential for harm. Then they ask why they were started on the medication in the first place. It entails having what I call a “sense-making conversation” with patients, and we worked to develop scripts for those conversations. We suggest saying things like, “Well you know we used to think these medications were safe. We now know they are not. There’s new evidence that these medications probably are not as safe as we thought.” So, you blame the medication and don’t blame the retiring provider.
BT: Historically, older patients are reluctant to have these shared decision-making conversations. Do you have any tips on engaging older adults in such conversations?
Dr. Parchman: It usually requires several visits. You have to build a relationship and frequently you find yourself in a position of saying, “OK, let’s not upset the apple cart today. We will give you enough to last you for another month or two. But, I need to see you back, and we need to continue this conversation. In the meantime, I want to give you some materials for you to read and think about and then we can talk about some options for your care.” The number one message is “I am never going to abandon you as a patient. I just want to make sure that you’re safe.”
BT: Can you share any insights from your practice facilitators, who need to convince clinicians to take the time to have those conversations?
Dr. Parchman: To have a conversation with the patient, you don’t have to go into a 20-minute long conversation. The other thing is, not to put it all on the shoulder of the prescriber. We train medical assistants and nurses on how to have these conversations with patients so everybody on the team is on the same page. (Find these tools here.)
BT: Is there any additional advice you’d like to offer?
Dr. Parchman: Be patient. This work takes time.
Conversation Series: Trauma and healing in the wake of the COVID-19 pandemic
Kathleen Noonan, CEO of the Camden Coalition of Healthcare Providers, and Daniel Wolfson, MHSA, executive vice president and COO of the ABIM Foundation, discuss trust and its relationship to trauma and healing in the context of the COVID-19 pandemic.
Previous Webinars:
- Conversation Series: Distributed, decentralized and digitally-enabled care
- Public Agenda is building trust with patients
- Conversation Series: COVID-19’s impact on trust
- Introducing the Building Trust Initiative
- Vaccine hesitancy impacts on state and local vaccine planning
- Enhancing Influenza and COVID19 caccine uptake
- Tools for building institutional trust
- The evolving role of Community Health Workers as trusted messengers
Leading internal medicine organizations sponsor $400,000 grant program to build trust and advance health equity
PHILADELPHIA, November 1, 2021 – The Alliance for Academic Internal Medicine (AAIM), the American Board of Internal Medicine (ABIM), the ABIM Foundation, the American College of Physicians (ACP) and the Josiah Macy Jr. Foundation have announced a second round of grants for internal medicine residents and faculty members, designed to improve the quality of education and training and create a more trustworthy health system that serves everyone.
The first round of grants in 2020 brought in 170 applications, from which 32 projects at medical schools and training programs were selected. The grants, which totaled $287,500, include projects such as expanding community-focused health curriculum for primary care residents at Magnolia Regional Health Center/University of Mississippi Medical Center and developing a training program for medical residents to work directly with the Hispanic community at UT Southwestern Medical Center, among others.
For this second round of grants, sponsors are devoting a total of $400,000 to support new or existing programs that promote trust and create a more equitable health system by incorporating diversity, equity and inclusion (DEI) into the fabric of internal medicine and training. Inter-professional programs that incorporate members from across the care team will be preferred.
Specifically, sponsors are seeking proposals that (a) focus on providing training, skill and competency acquisition with the goal of promoting trustworthiness through equitable outcomes, or (b) focus on engineering care processes to promote trustworthiness through equity.
Examples of successful projects could include:
- Training programs that incorporate DEI, and in particular those that employ inter-professional education best practices.
- Quality improvement programs and program evaluations that advance trustworthiness through health equity.
- Ideas on building trustworthiness and psychological safety among teams, including an intentional focus on recognizing bias, lack of diversity and the barriers to being heard due to hierarchical structures.
- Innovative approaches to create collaborative partnerships between health systems and community-based service organizations in under-resourced communities.
- Approaches that foster and support diverse and equitable pathways into medicine and faculty and leadership positions.
Letters of intent for the second round of grants will be accepted through December 1, 2021 and selected applicants will be invited to submit full proposals early next year. Grants of $20,000 and $10,000 will be awarded in Spring 2022.
###
About the Alliance for Academic Internal Medicine
AAIM represents over 11,000 academic internal medicine faculty and administrators at medical schools and community-based teaching hospitals in the US and Canada. Its mission is to promote the advancement and professional development of its members, who prepare the next generation of internal medicine physicians and leaders through education, research, engagement, and collaboration. Follow AAIM on Twitter @AAIMOnline.
About the American Board of Internal Medicine
Since its founding in 1936 to answer a public call to establish more uniform standards for physicians, certification by the ABIM has stood for the highest standard in internal medicine and its 21 subspecialties. Certification has meant that internists have demonstrated – to their peers and to the public – that they have the clinical judgment, skills and attitudes essential for the delivery of excellent patient care. ABIM is not a membership society, but a physician-led, non-profit, independent evaluation organization. Our accountability is both to the profession of medicine and to the public.
About the ABIM Foundation
The ABIM Foundation’s mission is to advance medical professionalism to improve the health care system by collaborating with physicians and physician leaders, medical trainees, health care delivery systems, payers, policymakers, consumer organizations and patients to foster a shared understanding of professionalism and how they can adopt the tenets of professionalism in practice. To learn more about the ABIM Foundation, visit www.abimfoundation.org, connect on Facebook or follow on Twitter.
About the American College of Physicians
The American College of Physicians is the largest medical specialty organization in the United States with members in more than 145 countries worldwide. ACP membership includes 161,000 internal medicine physicians (internists), related subspecialists, and medical students. Internal medicine physicians are specialists who apply scientific knowledge and clinical expertise to the diagnosis, treatment, and compassionate care of adults across the spectrum from health to complex illness. Follow ACP on Twitter, Facebook and Instagram.
About the Josiah Macy Jr. Foundation
Since 1930, the Josiah Macy Jr. Foundation has worked to improve health care in the United States. Founded by Kate Macy Ladd in memory of her father, prominent businessman Josiah Macy Jr., the Foundation supports projects that broaden and improve health professional education. It is the only national foundation solely dedicated to this mission. Visit the Macy Foundation at macyfoundation.org and follow on Twitter at @macyfoundation.
Patient Advocate Spotlight: Tara Montgomery
Tara Montgomery is a trusted change leadership advisor and strategist who strives to connect the dots between healthy people and healthy democracies, bringing consumer and citizen perspectives to conversations about culture change in health care and other complex systems. Tara is driven by optimism about the power of collaboration to solve the world’s most challenging problems, having spent over two decades convening and partnering with US, UK, and international academic, cultural, scientific, and nonprofit institutions and leading strategic initiatives to advance public health, education, corporate social responsibility, and social change.
No posts found.
Patient Advocate Spotlight: Dave Ellis
Dave Ellis is a national leader in providing trainings and facilitating conversations on the lasting impacts of ACEs and generational trauma. He shares his expertise with the State of New Jersey and coordinates statewide work related to ACE’s.
No posts found.
Enhancing education, building trust and eliminating bias in urban and rural Mississippi
The University of Mississippi Medical Center (UMMC) and Magnolia Regional Health Center (MRHC) both share the mission of decreasing the shortage of primary care physicians, reducing health disparities, and improving health outcomes throughout Mississippi.
In an effort to increase the number of residents and fellows training in primary care programs, Internal Medicine residencies at UMMC and MRHC have developed a partnership to expose trainees to both traditional academic and rural community-based graduate medical education. The intent is to expand the curriculum to strengthen patient-centered relationships as a core feature through a focused emphasis on didactic and clinical activities. This project strives to eliminate health disparities among Mississippians based on race, geography, income or social status.
Project initiatives include:
- Creating new educational activities and partnerships with both non-profit and privately funded organizations to enrich learner exposure to patients.
- Expanding primary care resident curriculum, including a series of community-focused educational health topics and interactive lecture series, with input from various stakeholders from the community and other health care workers.
- Educating students, residents and nursing leaders at local neighborhood centers, clinics and health fairs. The collaboration will focus on patient mistrust and physician bias, presented through a series of lectures, reflective narratives and community engagement activities.
Program quality and efficacy will be assessed by comparing patient assessments between residents actively involved in the program and those who are not. “Mississippi is the state known for having some of the worst health outcomes. We thought it would be great to have residents out in the community [in patients’ homes and at community events] to see if there are improved health outcomes. Getting residents out into communities where patients live will help to restore trust,” said Margaret Hayes Baker, MD, Program Director, Internal Medicine, MRHC and Director, Magnolia Hospitalist Group.
This project aims to strengthen the doctor-patient relationship by building trust with patients and decreasing bias in trainees. Project leaders will also measure the program’s impact on retaining primary care physicians to practice in Mississippi after training.
“By accomplishing each of these outcomes, we will impact the health care of Mississippians by increasing the number of primary care physicians who are well-trained in delivering safe, equitable care to our diverse patient population,” said Baker.

