Category: Guest Blogs
An exercise in trust
My passion for running began as a means to an end. At the time I started running, I was a wrestler, and I ran as a way to build endurance and control weight. But over the years, things changed. This means to the end became the sustaining quality and foundation for my physical activity, and remains so some 30 years later.
Running requires consistency, support through rest and good nutrition, and the discipline to keep putting one foot in front of the other in a rhythmic but often mundane process. In many ways, it’s a lot like what I’ve experienced as we’ve worked to pursue a culture of trust at the American Physical Therapy Association during my first four years as chief executive officer.
Trust is a term you hear a lot in organizational settings. At a recent association leadership conference, one speaker described trust as jet fuel; another described it as “the core competency of leadership.” Trust, in other words, was a resource, or a skill that could be honed. Or maybe, somehow, a little of both.
I think those experts missed the fundamental properties of trust. Trust isn’t something to be expended, or a set of techniques to be applied to situations — it’s a process, a practice, a pursuit. Trust isn’t a business book chapter or PowerPoint buzzword that should be covered before moving on to the next topic—trust is an ongoing exercise that empowers organizational and individual fitness.
Both at my association’s level and for me as an individual, exercising trust has become a daily pursuit to seek a higher level of functional fitness. It’s like running: it has to be consistent in approach, supported in behavior, and disciplined in application.
And there are no shortcuts. If we could’ve purchased hi-test trust fuel or sent staff to a continuing education weekend for a certificate in trust, we would’ve been all-in. Instead, we knew we’d have to commit time, effort, discipline, and a posture of learning. We needed to learn to walk the walk and talk the talk of building trust. Trust would become a form of exercise, with the goal to gain flexibility, strength, and endurance to enhance the credibility of the organization to its community of stakeholders.
Trust isn’t something to be expended, or a set of techniques to be applied to situations — it’s a process, a practice, a pursuit.
However, before we could begin our exercise program, we needed to take stock of our current state of fitness. And we needed to gain insight into the best ways to move. We needed to reflect, reconcile, and then seek results.
Our reflecting began with an effort to better understand the perspectives of our stakeholders and the perceptions of potential partners. We engaged outside consultants who offered us sound, research-driven information on the perspectives and perceptions of key audiences. Those insights helped us build a strategic plan and new brand promise that seeks to close our trust gaps, including becoming a more relevant, credible, and consistent source of information, programs, and services.
Reflection led to reconciliation. As an organization, APTA had grown through advocacy and the advancement of science that confirms the efficacy of physical therapy. The profession had achieved independence in its educational enterprise including accreditation, and it has become a recognized health care profession at the state and national levels. But that growth came at a price: the erosion of trusting relationships with many of the health care professions with which we must collaborate to best serve our patients. We needed to reconcile our hard-fought independence with the greater value of interdependence, and we needed to embrace trust as the means by which we could achieve that optimal goal. This required some long-overdue conversations with organizations that were opponents in past turf battles, to move from a posture of competition to collaboration.
But ultimately, we needed to deliver results. Reflection gave us a playbook and a brand that we would seek to deliver. Reconciliation engaged other organizations, shifting foes to friends in the pursuit of shared goals. Results are the practices, programs, and outcomes that will validate our exercise program.
Those results are emerging. The one thing we have discovered so far is that exercising trust is worth the effort. We are improving, learning, and seeking new strategies of engagement with stakeholders, from patients to other professional societies. This is how we grow and improve our fitness for service, and our fitness to deliver the best possible care.
As we grapple with the future of health care, we can be certain that trust will play a central role at all levels. We can no longer rely on white-coat symbolism. We need to turn to a pursuit of partnerships with individuals in care, and with communities impacted by what we do.
Building trust by identifying, scaling, and sustaining successful practices will require the rhythmic process of putting one foot in front of the other, over and over and over again. The commitment to inclusion, learning, and communicating with others necessitates that we don’t think of trust as a commodity, but as a way of doing—a steady, consistent, disciplined effort to stay fit, healthy, and prepared for the challenges ahead.
Find harmony in the hospital
Several years ago, I was invited by a large hospital system in the Midwest to facilitate a conversation between a group of physicians and nurses who, according to the vice president for clinical affairs, “were at war with one another.”
The origins of the war were murky, but there were frequent complaints from both sides about a lack of trust and conflict between the two groups that stretched back years. At the beginning of the day, and as people were milling around in their respective tribes, the VP pointed out one nurse and one physician to especially watch out for, “… because whenever they’re together distrust and conflict aren’t far behind.”
These two warring professionals became my “canaries in the coal mine.” If they could somehow manage to find common ground, anything might be possible.
After a short introduction and description of how using an us versus them logic was ultimately enervating, eroded trust, and was a potential source of burnout, I invited the group to think about the things they loved about their work and/or lives, and to speak them into the circle in which the room chairs had been arranged.
Creating trust among medical professionals is not only possible, it is the bedrock on which our day-to-day work is based.
People talked about aspects of their work they loved, their children, their families and friendships, hobbies, and the like. When it came to the physician I’d been warned about, he started off by saying, “You know, I’ve been practicing medicine for the past 30 years and I still enjoy it somewhat, but what I really love is playing the organ in my church. I live for Sundays when I can get lost in the music and the sound of the organ in such a special space.”
The nurse, who was the next to speak, turned and said, “That’s really amazing because in the 25 years that we’ve worked shoulder to shoulder together, I never knew anything that really grabbed you outside of work.” With misty eyes she went on to say, “Like you, I enjoy my job as a nurse, but to me at this point it’s just a job. What I really love, is playing the organ in my church, and for exactly the same reasons!”
There was a brief silence followed by smiles and clapping in appreciation of the moment that had just occurred. The nurse and the physician, too, were smiling at each other, recognizing at that moment, in fact, they were more alike than different. More importantly, they each took a risk and trusted a process designed to tap into what we’re like when we’re at our best.
Throughout the day, during small and large group exercises, there was a noticeable shift in the tone and content of conversations within and between the two professional groups. It was as if what had happened to the two “canaries” had come home to roost as a model for how to take risks, speak from the heart, and trust in one another’s good will and intentions.
Creating trust among medical professionals is not only possible, it is the bedrock on which our day-to-day work is based. It is also an antidote to the isolation and fear that so many health professionals feel and that threaten to undermine trust in one another and of our institutions.
Frankel is Professor of Medicine and Geriatrics at Indiana University School of Medicine where he directs the ASPIRE Fellowship, (Advanced Scholars Program for Internists in Research and Education). He is also a senior scientist at the Regenstrief Institute, Indianapolis, and holds an appointment in the Education Institute at the Cleveland Clinic.
Trust should be a two-way street
It took me a long time to find a doctor that actually believed me. I was walking around in pain for five years because nobody believed me. Why did I have to suffer for so long? Why did no doctor believe the pain that I was in?
Person with Medicaid in her 40’s; Native American; Minneapolis focus group
When researchers and clinicians talk about trust in health care, they are almost always talking about patients’ trust in physicians. But patients can suffer when doctors do not trust them, as the woman quoted above explained in a focus group that Public Agenda conducted for a project about making care more patient-centered, in partnership with AcademyHealth and the Robert Wood Johnson Foundation (RWJF).
In October 2020, Public Agenda released findings from representative surveys that compared the perspectives of people insured by Medicaid and the primary care physicians who treat them about what can build and damage mutual trust. The report, titled “A Two-Way Street: Building Trust Between People with Medicaid and Primary Care Doctors,” was one of eight projects about building trust funded by RWJF.
Public Agenda’s survey findings show that most people with Medicaid and most primary care physicians who treat them believe that it is important both for doctors to trust their patients and for patients to trust their doctors. The research also found that most of these physicians and most people with Medicaid think doctors and patients should be equally responsible for building trust
As a result of the trust, you have good outcomes because the patient will adhere to the regimen, will come back to see you, will trust your judgment. But you have to gain the trust.
Primary care physician in his 60s; white; New York City focus group
The research found that most primary care doctors (79 percent) feel that their patients with Medicaid are just as trustworthy as their patients with other types of insurance. But if someone anticipates that doctors will mistrust them, it could be hard to forge healthy doctor-patient relationships. In fact, only about half of people with Medicaid (46 percent) think that primary care doctors trust people with Medicaid as much as they trust people with other insurance. Twenty percent of them think doctors trust them less, and about one-third say they do not know.
Medicaid covers a relatively high proportion of Black and Latino/a Americans. Several people with Medicaid in focus groups described feeling mistrusted or disrespected by health care providers because of both their race and their insurance type:
Being on Medicaid is like a public kind of thing. I think that some doctors ain’t going to respect people who are on Medicaid like they do private insurance.
Person with Medicaid in his 50s; Black; New York City focus group
I think that African Americans at times were sort of looked at negatively, like we don’t care about our health. And then they see the fact that you might have Medicaid. I think sometimes it does factor into how they perceive you and how they treat you.
Person with Medicaid in her 40s; Black; Philadelphia focus group
What do primary care physicians say affects their trust in people with Medicaid? According to Public Agenda’s survey, primary care physicians trust people with Medicaid more when they are actively engaged in their care. For example, most primary care doctors (71 percent) also say they would trust someone with Medicaid more who told them about their goals for their health and well-being. When asked about the two most important things people with Medicaid can do to make doctors trust that they want to do what is best for their health, 56 percent of primary care doctors prioritize providing complete, honest information.
Trust-building behaviors that primary care doctors also prioritize include people with Medicaid having reasonable expectations about their care, following treatment plans and participating in discussions and decisions about their care. The behaviors that primary care doctors say can damage their trust include patients leaving out information, exaggerating symptoms and insisting on specific medications or treatments.
Because primary care doctors express more trust in people who play more active roles in their care, interventions aimed at building patient activation and engagement may have positive effects on providers’ trust in patients—an outcome that future research on those interventions should measure. Structuring primary care practices to provide the time and space for good communication can help create the conditions for mutual trust.
Primary care doctors who treat people with Medicaid largely understand that they need to trust patients in order to provide high-quality care. Do other types of medical providers understand this as well? To move health care away from paternalism and toward centering patients, more research and dialogue are needed about how providers’ trust in patients correlates with decision-making styles, safety practices and patient outcomes. More research and dialogue are also needed to explore variations in providers’ trust in patients comparatively across specialties, physician demographics and patient populations.
How can we ensure that doctors trust patients when they describe their symptoms, worries, behaviors and side effects? With rising COVID-19 cases and deaths, which disproportionately affect people of color, doctors’ trust in patients can be a matter of life or death. And with the prospect of a COVID-19 vaccine on the horizon, ensuring that people trust the information and interventions that their doctors are providing will be crucial to safeguarding public health and restarting the economy.
David oversees the development, management, and implementation of Public Agenda’s research projects and on collaborations with Public Agenda’s public engagement and higher education and workforce engagement departments. His research includes projects in health care, higher education, K-12 education and civic participation.
Rebecca works on all phases of Public Agenda’s research and evaluation projects including: project design, data collection, analysis, and reporting. She is experienced in a broad set of qualitative and quantitative research methodologies such as participatory design, surveys, individual interviews and focus groups.
The virus does discriminate
“The virus does not discriminate,” the infectious disease experts told us. As the COVID-19 pandemic reached the United States, that warning was issued with the best of intentions. If you search for that phrase today on Twitter, you’ll find the message being repeated, as public health officials implore all Americans to protect ourselves and others from the latest surge in cases of COVID-19.
From my home in Brooklyn, an early epicenter of the pandemic, it didn’t take long to wonder if something was awry with that message. At every turn, our understanding of COVID-19 and our response to it have been complicated by mixed and misleading messages. Science denial and political motives have introduced misinformation. At the same time, rapid shifts in evidence and knowledge have required new policies and messages. The combination of bad faith and emerging science has muddled public understanding and fueled mistrust. For some of us, mistrust is deeply self-protective. A history of medical exploitation and the systematic denial of access to the opportunities and social conditions that determine health gives millions of Black Americans cause to doubt that their lives really matter.
From mid-March through mid-April, as I sheltered safely in my apartment in one of New York City’s whitest, most affluent neighborhoods, I listened with fear and grief to the round-the-clock sirens from ambulances carrying COVID-19 patients to our local hospital. Yet few of my neighbors were among them. Apart from those who are frontline health care professionals, the majority of my neighbors are not essential workers. They aren’t riding the subway to work. Most of my neighbors, based on their demographics, are the kind of people who have good health insurance and paid vacation and sick days and cars and gym memberships and healthy food deliveries. There’s a good chance that they don’t know anyone who has been incarcerated. It’s unlikely they have had negative experiences with the police or medical professionals.
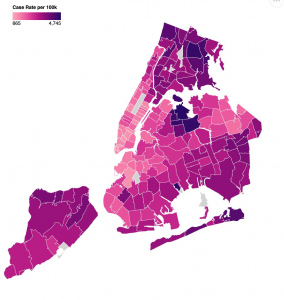
When New York City started to release data on COVID-19 cases, hospitalizations, and deaths by race and ethnicity (in April) and then by zip code (in May), the zip code covering most of my neighborhood (11215) stood out on the color-coded map as a poignant patch of pale pink, representing the lowest infection rate in Brooklyn. I don’t know if the graphic designers chose this palette intentionally, but its symbolism was not lost on me. In New York, the impact of the virus on people of color and residents of majority-Black and Latinx zip codes has been particularly devastating. Our COVID-19 maps paint a graphic picture of Blackness as a co-morbidity here and across America (when data is made available—a problem in itself). They awaken my understanding of why so many people cannot trust experts. The experts were wrong: the virus does discriminate. The virus discriminates not because of biology, but because we as a society allow it to. They deepen my understanding of why so many people do not trust our country’s leaders. If we cannot trust in our systems to protect our most vulnerable people from a pandemic virus, we cannot trust them at all.
For several years, I’ve been participating in efforts to help build and rebuild trust in health care. Most of my work on trust has been at the levels of interpersonal relationships, team behaviors, and organizational cultures. When I’ve looked at the systemic level, the focus has leaned towards effective public engagement or solutions for repairing the health care system itself. We’ve assumed in good faith that if we rebuild trust in health care piece by piece and publish enough respectable articles about best practices and the role of professionalism, we will catalyze change. Those strategies are still meaningful, but they aren’t enough anymore. COVID-19, with its devastating impact on Black and Brown people, is evidence enough that wider systems of injustice in America not only drive bad health outcomes but also betray our founding values. What if we admit that the distrust in our country’s institutions is warranted? What if we accept that our failure to mitigate COVID-19 is not only a consequence of inequities in our health care system, but is so enmeshed in systemic injustice that we cannot fix it as if it were a quality improvement initiative?
By June, Brooklyn’s Grand Army Plaza, the gateway for thousands of ambulances on their final approach to our local hospital, had become the gateway for thousands of mask-wearing protestors to join the Black Lives Matter marches. When the sound of sirens was replaced by the sounds of chanting and police helicopters, it was a call to action for all of us who are serious about rebuilding trust. It demands that we listen better. Health equity cannot happen until we reckon with systemic racism. Trust cannot be won until we earn it at the most fundamental level. If we want to do better, we need to rise to the challenge of rebuilding our country based on social, racial, and economic justice. It may feel uncomfortable to those of us who have spent our lives believing that professionalism required us to politely avoid crossing the boundary between science and politics. But the pandemic compels us to do just that. It’s time for physicians and health care leaders to use our privilege to dismantle the unhealthy systems that undermine our national wellbeing. This is how we will earn trust.
Tara Montgomery is Principal at Civic Health Partners, an organization she founded after 15 years leading Health Impact at Consumer Reports. As a coach, speaker, and writer, she guides leaders through the discovery of ethical solutions and trust-building strategies that integrate empathy and evidence.
Amidst the pandemic, building trust between patients and health care providers
COVID-19 has exposed many frailties in the American health system but has it done some good for Americans’ attitude towards it? A recent Gallup poll shows that over 90% of Americans approve of health care providers’ handling of the COVID-19 response. With daily evening cheers and other signs of enthusiastic support, Americans’ support for health care professionals may be at an all-time high. While Americans may praise the efforts of individual caregivers amidst the pandemic, we know from survey research that Americans’ trust in the health care system has been eroding for many years. If we hope to maintain this newfound appreciation for health care providers, we must take a good look at our system and how we can create an environment conducive to trust.
The ABIM Foundation’s Building Trust initiative seeks to elevate the importance of trust as an essential organizing principle to guide operations and improvements in health care. To support the initiative, Public Agenda has conducted interviews with several consumer and patient experts and advocates about opportunities they see for advancing trust in health care. This will provide the initiative with actions and practices that promote patient trust in their clinicians and the health care system.
One theme that has emerged so far in the interviews is the importance of ensuring that health care facilities are truly accessible. It is hard to trust someone if they don’t devote effort to making their space accommodating to you. Maya Sabatello LLB, PhD, Assistant Professor of Clinical Bioethics in the Department of Psychiatry at Columbia University College of Physicians and Surgeons with decades of experience as a disability rights advocate and scholar says that we need to confront our “generalization of needs” concerning accessibility. “The ramp isn’t enough,” she says. “It doesn’t help a deaf person. Think about the postings in medical institutions. They rarely include braille.” These physical barriers can make patients with disabilities feel unwelcome and reinforce the exclusion they may experience from society at large.
Even if people aren’t overtly experiencing discrimination, they are still guarded.
Kellan Baker, MPH, MA
Another theme that has emerged is the need to not only remove physical barriers but actively create welcoming spaces for marginalized patients. Kellan Baker, MPH, MA is the Centennial Scholar in the Department of Health Policy and Management at the Johns Hopkins Bloomberg School of Public Health. As a transgender man, he can attest to the pervasive discrimination that LGBTQ people, especially transgender people face, even in health care settings. “Even if people aren’t overtly experiencing discrimination, they are still guarded.” Baker says that to create trust, robust nondiscrimination policies must be created and prominently displayed in the waiting room area. He also noted the need for respectful and inclusive data collection in healthcare settings about patients’ sexual orientation and gender identity. Health care staff must also know how their behavior creates either a welcoming or hostile environment. “Cultural competency training [must] be made available not only to providers, but to all staff who patients may interact with.”
Over the coming months, the ABIM Foundation, Public Agenda, and the National Patient Advocate Foundation will be diving deeper into this question of what it takes to build sustained trust in the health care system from the perspective of patients, consumers and caregivers. To inform this work, we’ll be talking with many other stakeholders about what’s working all over the country and what people want to try. As we step into an uncertain future with COVID-19, this knowledge can help us meet the challenges of the pandemic and understand how to seize the opportunities to build greater trust.
Treston Codrington is the Public Engagement Associate at Public Agenda. He is a writer, community organizer, and proud native of Brooklyn, New York. With a wealth of local and international engagement experience, his goal is to bridge the divide between communities, scientists, and policy-makers and help facilitate co-productive processes with these stakeholders to improve our world.
Matt Leighninger leads Public Agenda’s work in public engagement and democratic governance and directs the Yankelovich Center for Public Judgment. Matt is a Senior Associate for Everyday Democracy and serves on the boards of E-Democracy.Org, the Participatory Budgeting Project, the International Association for Public Participation (IAP2USA), and The Democracy Imperative. In the last two years, Matt developed a new tool, Text, Talk, and Act, that combined online and face-to-face participation as part of President Obama’s National Dialogue on Mental Health. He is author of The Next Form of Democracy (2006) and co-author of Public Participation in 21st Century Democracy with Tina Nabatchi.
Grief and gratitude
“Covid-19 was initially hailed as the great equalizer…but it arrived in America and immediately became American: classist, capitalist, complacent.” Teju Cole, “We can’t comprehend this much sorrow.” New York Times, May 24, 2020
I have had the opportunity to deeply listen and pay attention to my own and many health care providers’ intense grief over how our health care system has failed people of color. None of this is new; it has merely been intensified and unmasked in the pandemic. To be clear, my experiences come as the result of a lifetime of immense, largely unearned, privilege – professionally, socioeconomically and racially.
I hear this grief because of my role in helping organizations develop and sustain peer support programs. Since the pandemic began, I have provided virtual peer support to dozens of peers. Many of them share their grief and anger over the widespread structural inequities that our society has ignored and sometimes actively perpetuated. They speak about their mistrust of a health care system that has prevented and at times even co-opted us into propping up structures that prevent us from providing the kind of care we entered the profession to provide. They voice anger and mistrust of government and leaders for their lack of transparency and ultimate failure to provide resources that are needed to protect our particularly vulnerable populations.
As with many intense and complicated life challenges, my personal experience of these times holds a paradox: grief and gratitude.
As with many intense and complicated life challenges, my personal experience of these times holds a paradox: grief and gratitude. I feel grief and anger over our failures and the resulting burdens that have been placed on so many marginalized communities. Grief and guilt for all that I did not do and did not see. Gratitude for activists both within and outside of health care who have long been working towards a better way, and to those activists and many more of us who are now redoubling or joining that work. Gratitude for my opportunity to learn and do more. Gratitude for those health care leaders who are now listening and acting on behalf of those marginalized groups. And gratitude for the honesty and intensity of caring I have been privy to hearing in providing emotional support for health care providers, as they share their depth of caring, helplessness and hopefulness.
I have long trusted in the overall integrity and caring of my peers. Trust in government and health care leaders has been significantly damaged and will need to be rebuilt. I feel an awakening of possibility.
Jo Shapiro, MD, FACS is an associate professor of Otolaryngology-Head and Neck Surgery at Harvard Medical School and a consultant for the Massachusetts General Hospital Dept of Anesthesia, Pain and Critical Care. She is Senior Faculty for the Center for Medical Simulation in Boston and was the founding director of the Center for Professionalism and Peer Support at Brigham and Women’s Hospital.
Check-out etiquette
I had been building a therapeutic relationship with a patient over her last three visits. We bonded over being newly married, our mutual excitement about married life and the varying definitions of cleanliness partners could have in a relationship. During this visit, she had been experiencing abdominal discomfort and nausea. A simple test revealed she was pregnant.
The patient looked stunned and began to cry softly. She had previously told me that she and her husband were struggling financially and were not planning to become pregnant for several years. We had discussed contraception at her last visit and she was considering several options. She explained that she had been thinking seriously about contraception and was frustrated that she had not moved forward with an intrauterine device (IUD) prior to becoming pregnant.
As a trainee, I am constantly working on the therapeutic relationship which begins with trust. I learn every day the impact that the small things that I do have on my patients.
Through our previous interactions I had a sense that what she needed after receiving this news was time to process. We initially sat in silence and I held her hand. I then stated that I was here to listen and help support her. I was not there to judge her and would give her all the information to make whatever choice was right for her. At that moment I felt as though our therapeutic relationship, which initially started with a bond over shared lived experiences, had developed into a trusting patient/physician relationship.
She felt comfortable telling me that she wanted to terminate the pregnancy and would like an IUD placed after the procedure. I included the address for Planned Parenthood in her after-visit summary along with a note to my checkout staff to assist in scheduling the IUD placement appointment.
She later told me that when she went to check out, the clerk was adamant that she schedule a follow-up appointment for the IUD placement. This was an uncomfortable question for her and she felt pressured into explaining the need for an initial appointment at Planned Parenthood. She felt embarrassed and upset.
I have reflected on this many times since it occurred. She trusted that I understood the sensitivity of the matter. In my effort to be helpful and efficient, I feel damage was done to our relationship because of the way the checkout process unfolded. I have thought about various ways in which I could have made this experience easier on her, including asking her to contact the clinic when she felt she was ready for contraception or adjusting my communication to my checkout staff to include a note about the sensitive nature of this visit. Fortunately, the patient did come back for follow-up so we have a chance to continue to build our therapeutic relationship.
We all strive to do our best for the patients that we serve. As a trainee, I am constantly working on the therapeutic relationship which begins with trust. I learn every day the impact that the small things that I do have on my patients. I am humbled in this endeavor and hope that the hard lessons are few.
Adetoye is a third-year resident in Family Medicine at Michigan Medicine, the University of Michigan Health System.
Patient Portal: A platform for trust
As a physician, I use the electronic health record (EHR) to educate patients and empower them to make knowledgeable decisions about their care. However, as a daughter of elderly parents with complex medical conditions, the EHR takes on a more personal meaning – it’s my lifeline to their care team, and it enables me to coordinate their health care needs.
There’s a term for those of us in our 30s to 40s who are raising children while caring for elderly parents: the Sandwich Generation. As this generation grows, so does a unique subgroup of “long-distance” caregivers – those of us juggling medical decision making remotely. For me, the EHR and, more specifically, the patient portal allows me to fulfill this critically important role in my parents’ lives – from 2000 miles away.
Via the patient portal, I can order, pay for and arrange home delivery of their medications. I can communicate every six weeks with their geriatric pharmacist about the impact of tweaks in their medication management. I can schedule three-way phone or even video conferences with my dad and his geriatrician.
By developing platforms that are grounded in the patient and family experience, we can make real strides toward improving engagement, trust, and the overall experience of care.
The patient portal enables me to communicate, advocate, and facilitate on behalf of my parents. More importantly, I’m made to feel my engagement on the portal is positive, and that feeling promotes trust – my trust in their care team, the care team’s trust in me as their partner, and also my parents’ trust and confidence knowing we’re all working together.
That being said, technologies such as patient portals and EHRs can be far from perfect. On my parents’ portal, a change to the pharmacy interface left me struggling to refill medications for nearly a half hour, which was worsened by the lack of a tech support option. A search for their annual residential care facility form unhelpfully generated hundreds of unrelated results, and still didn’t provide a way to submit it online to medical records. And then there are small things, such as that I can only know what their physician looks like; the rest of their care team (and my parents) don’t have the ability to upload their headshots. That might seem trivial, but putting a face to the pharmacist I speak to every six weeks would make me feel more connected to the team.
For patient portals to facilitate real meaningful use, they must evolve to meet the needs of patients and their families. Technical support such as a live chat feature, as well as advance notice of layout or functionality changes, can help alleviate user frustration.
Ongoing end-user input from patients and caregivers is critical – both in the form of real-time feedback about the user experience and through dedicated organizational engagement with patient and family advisory council representatives to seek their perspectives on the use of technologies such as EHRs. By developing platforms that are grounded in the patient and family experience, we can make real strides toward improving engagement, trust and the overall experience of care.
Lollita Alkureishi is a board-certified pediatrician with UChicago Medicine and Associate Professor in Academic Pediatrics at the University of Chicago & Clerkship Director at the Pritzker School of Medicine. Her goal is to provide continuity of care and preventive health care services for medically underserved youth. She was among eight winners of the ABIM Foundation’s Trust Practice Challenge in 2019.
Trust as an antidote to the viral spread of medical misinformation
The existence of medical misinformation is palpable for anyone scanning recent news headlines. Journalists and commentators often point to the spread of misinformation as a regular aspect of contemporary life, as we have seen in reporting on the novel coronavirus, which causes COVID-19. Faced with emerging and continued threats to public health and the simultaneous specter of patients being misled by misinformation, some health care professionals are frustrated and wonder what they can do to help.
At Duke University, I recently spent time talking with health care professionals in a workshop for the Duke AHEAD program that I organized with Dr. Jamie Wood, a medical education faculty member at Duke’s School of Medicine. Many participants had stories to tell about patient encounters with misinformation. Participants also were eager to talk about hypothetical scenarios we introduced as prompts to consider how we might optimally talk with patients about misleading information they reference, e.g., regarding an untested treatment for cancer.
We do not have the time or resources to argue against every false claim to which patients are exposed, but we do have opportunities to build and reinforce trust by acknowledging and listening to patients.
In many instances, health care professionals’ first response is to generate a reasonable counterargument regarding misinformation, e.g., “my argument to them would be…” That well-intentioned response to patients, however, misses an important opportunity that could be central to our systemic response to the spread of medical misinformation.
What if our first response to patients who reference clearly problematic claims was to ask: “Why are those claims important to you, and what concerns or questions do you have about your health?” We do not need to validate false claims in order to acknowledge and validate our patients’ interest in well-being. If we can take a deep breath and focus on listening rather than counterarguing, we often can find opportunities to redirect patients to credible sources of information.
At a system level, we also could better monitor patient encounters with misinformation and develop easily accessible information sources that respond to the questions those encounters raise, rather than simply bemoan the falsehoods. We could be systematically tracking patient questions and learning from those questions to craft educational resources for communities. In this way, patient encounters with sensational misinformation could help crystalize their questions and concerns (even if at the same time also offering a frustrating distraction), which means that with the right monitoring and learning tools we could improve patient health education.
We do not have the time or resources to argue against every false claim to which patients are exposed, but we do have opportunities to build and reinforce trust by acknowledging and listening to patients. Such trust could inoculate against future acceptance of medical misinformation by encouraging conversations. From this perspective, patient references to misinformation in the clinic can be a victory of sorts if we consider that the alternative is patient refusal to show up at all or reluctance to mention their concerns in the first place.
Brian Southwell is Senior Director of the Science in the Public Sphere program at RTI International and Adjunct Professor and Duke-RTI Scholar at Duke University. He has written and edited numerous articles and books on misinformation and public understanding of health, including Misinformation and Mass Audiences (University of Texas Press). He also hosts a public radio program called The Measure of Everyday Life for WNCU.
To heal, first build trust
My first job in health care was at the Harvard Square Homeless Shelter. Together with other energetic undergrads, I helped raise money to start a clinic inside the shelter.
I thought the homeless people who came to the clinic would immediately gravitate to us and the services we provided. But they didn’t. In fact, I remember one patient, whom I’ll call “Fred,” regarded the clinic with outright suspicion. For the life of me, I couldn’t figure out what we were doing wrong.
Years later, I came to understand that, though we’d built a great facility, what we’d failed to build was trust. Men and women like Fred had been bounced around from one end of the health system to the other, receiving fragmented care from any number of providers who treated the ailments in front of them and then sent them on their way. These anonymous clinicians failed to build trust with Fred. So he viewed them — and the whole health system — with suspicion.
We can build trust by doing what we say we’ll do, by being responsive, by being transparent, and by being authentic.
I think about this experience a lot these days. We live in a time when the democratization of information is eroding people’s trust — in one another, in expertise, and in institutions. As my experience in the clinic shows, as physicians, we can’t hope to heal people who don’t trust us.
That’s a problem because trust is fundamentally about longitudinal relationships that are developed over time. And yet, in our fragmented, fee-for-service-based health system, patients often see a multitude of clinicians, with whom they spend very little time. At best, this system undermines continuity of care. At worst, it undermines trust.
So it’s incumbent on us to go against the grain and take meaningful steps toward trust-building. We can build trust by doing what we say we’ll do, by being responsive, by being transparent, and by being authentic.
Sometimes the steps are harder. Sometimes the best way to build trust is to work closely with our patients to get to the root causes of their ailments, whether those causes are health-related, behavioral, economic, or social. It’s easy to write a prescription for an illness. It’s harder to talk to a patient about how they came to contract that illness, or why it might be recurring.
In the years since I worked at the homeless clinic, I’ve made it my priority to take the time to listen to my patients, to answer their questions, and to understand how my actions look from their points of view. As clinicians, we may not always have all the answers, but the least we can do is be present and intentional in our efforts to establish and nurture trust.
That’s not always easy. But as I learned from patients like Fred, it is always necessary.
Sachin H. Jain, MD, MBA, FACP is CEO of SCAN Group and Health Plan and Adjunct Professor of Medicine at Stanford University School of Medicine.

